According to a recent report by the Stanford-Lancet Commission on the North American Opioid Crisis, “more than 600,000 people in the USA and Canada have died from opioid overdose since 1999, and a staggering 1.2 million more are estimated to die due to overdose by 2029.”
The opioid crisis has reinforced hard lessons learned in earlier health crises. Chief among those is that we need multiple strategies if we are going to be successful in saving lives by reversing overdoses and treating opioid use disorder. Having just one option to fight back will not work as the crisis will evolve, and indeed, it already has.
When the opioid crisis began, it was primarily driven by heroin and oxycodone, but now illicit fentanyl pouring across our borders has quickly become a leading contributor to overdoses and deaths. Over time, the potency of opioids has increased—and now illicit fentanyl is contaminating much of the illicit drug supply, bringing us to the current situation. Illicit fentanyl is substantially more potent than other opioids, and when people ingest it, they often do not have sufficient tolerance to prevent respiratory depression or apnea – leaving only minutes at best to reverse the respiratory depression before brain damage or death results.
As two skilled professionals on the front lines of this crisis, here’s what we know after decades of fighting this battle.
One of us is an addiction medicine physician, the other, a recovering heroin addict, who is now reversing overdoses as a firefighter and paramedic and is training thousands of people to carry and administer naloxone.
Recently, one of us – Theo, a Los Angeles firefighter – was working the night shift when called to a scene where a 22-year-old man was found unresponsive, showing all the signs of a severe opioid overdose.
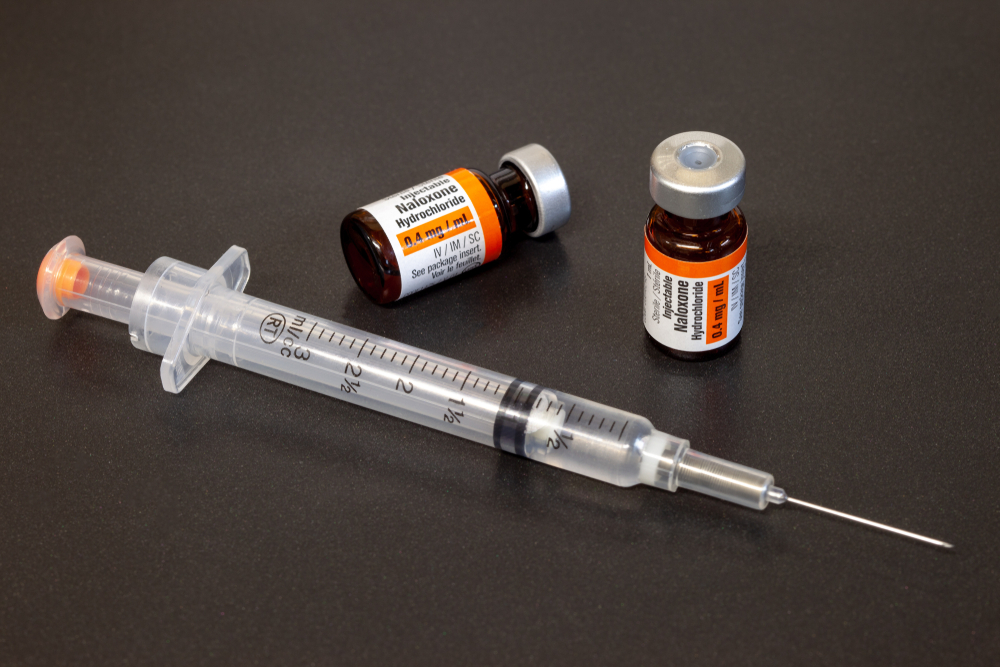
Despite being administered two doses of the standard 4 milligram (mg) nasal dose of naloxone, his condition barely improved. In a race against time, we administered additional intravenous naloxone just to get him to breathe again.
With each passing second, this man’s chances of survival dwindled. While we were able to revive him, the naloxone administered initially was not enough, and he suffered an anoxic brain injury and will now require a ventilator for the rest of his life. All of us involved wanted a better outcome, and we knew that providing a stronger dose of naloxone in the first administration could have made the difference.
Sadly, this experience is not uncommon and highlights the inadequacy of our current resources and education. As the opioid crisis has evolved, fentanyl and its analogs present challenges that our current standard of care cannot fully address.
In 2022, the most recent year with complete data reported by the Centers for Disease Control and Prevention (CDC), more than 109,000 people in the United States died of drug overdoses, the majority of which were opioid overdoses. In emergency situations, a quick response can make the difference between a person surviving an opioid overdose or suffering sudden death or lifelong brain damage.
Those like us on the frontlines—physicians, first responders, parents, and school nurses, among others—know there’s no one-size-fits-all approach in these emergencies. This is why many public health officials, from the White House to harm reduction organizations, have called on the industry to produce different strengths of naloxone products. They have responded.
However, we’ve become concerned about recent news stories claiming that a 4 mg dose of intranasal naloxone is better than an 8 mg dose.
These stories are based on a report recently included in CDC’s Morbidity and Mortality Weekly Report (MMWR). Importantly, this report was not peer reviewed. In fact, a disclaimer was added to the report saying it was not considered research. What we know from the long history of medical science, drawing broad conclusions from a report like this that is anecdotal at best, as some already have, creates dangerous misinformation. This misleading narrative could have a significant impact on whether people live or die.
First, while this report draws on filings by several New York State Police troops, there was no discussion of the total naloxone doses provided to each patient or the timing between doses (law enforcement is known to give repeat doses without waiting 2-3 minutes). This is an important factor when trying to compare 4 mg to 8 mg naloxone. In fact, we know from peer-reviewed studies that people overdosing often need more than 4 mg to be revived, sometimes even more than 8 mg.
Second, this report was limited to medically trained police officers. However, as we see on the frontlines, there are many incidents where non-medically trained bystanders, teachers, acquaintances, or parents can and should help administer naloxone. In these situations, thinking that a 4 mg dose is sufficient could risk the person’s life.
While we must always review the techniques and treatments used to treat people, especially in life-or-death situations, we should not draw new conclusions until we have peer-reviewed data. The New York State Police’s report confuses rather than clarifies the most important questions confronting non-medically trained people who are trying to save lives in these emergencies: How long should the average person wait to provide the next dose? What signs should they look for? In fact, a recent FDA-funded peer-reviewed study examining dosing strategies concluded, “These findings suggest that further evaluation of community naloxone dosing strategies is warranted.”
Higher-dose naloxone ensures a swift and effective response to overdoses involving today’s more potent opioids and facilitates the return of spontaneous respiration. Many communities, including first responders and doctors like us, prefer higher doses of naloxone to give us the best chance of quickly and successfully reviving someone experiencing an opioid overdose.
Reports like the one published in the MMWR do not advance what should be our top public health message: the opioid epidemic is changing and impacting diverse communities with illicit fentanyl on the rise, so it is imperative that people carry naloxone and have access to more options not fewer.
With more information and a range of naloxone dose options, we can finally bring down the number of Americans killed or permanently injured by opioid overdoses every year. Then, there will be fewer stories of overdose victims with permanent brain damage requiring a ventilator for life and more stories of people in recovery who now save lives as a firefighter and paramedics.
David I. Deyhimy is an addiction medicine specialist and anesthesiologist dedicated to helping those suffering from drug addiction and preventing overdose deaths from opioids. He is the founder and medical director of MYMATCLINIC (also on Facebook, YouTube, and Instagram @mymatclinic), specializing in treating and prescribing medications for opioid use disorder (MOUD). Additionally, he serves as the chief medical advisor for End Overdose, a nonprofit dedicated to preventing opioid overdose deaths through education, training, and distribution of overdose reversal resources. Dr. Deyhimy also holds the position of medical director at The Solace Foundation of Orange County, the first naloxone distribution program in Orange County with over 2200 documented opioid overdose reversals. Moreover, he acts as a medical advisor for health care companies focusing on treatments and technologies for opioid use disorder and preventing overdose death. A firm believer in medical research and evidence-based treatments for drug addiction, he has helped thousands of patients improve their lives with medical treatments, education, and behavioral change.
Theo Krzywick is a paramedic.